What Causes Lupus – Inflammation Driven By Toxins
If you want to know what causes lupus, evidence suggests that genetics combined with environmental factors are to blame. Lupus is a chronic autoimmune disease that results in inflammation which leads to damage to the body’s organs and tissues. It affects more than 1.5 million Americans, with women being most likely to experience symptoms.1 Inflammation contributes to all autoimmune conditions, including lupus.
What Are The Symptoms Of Lupus?
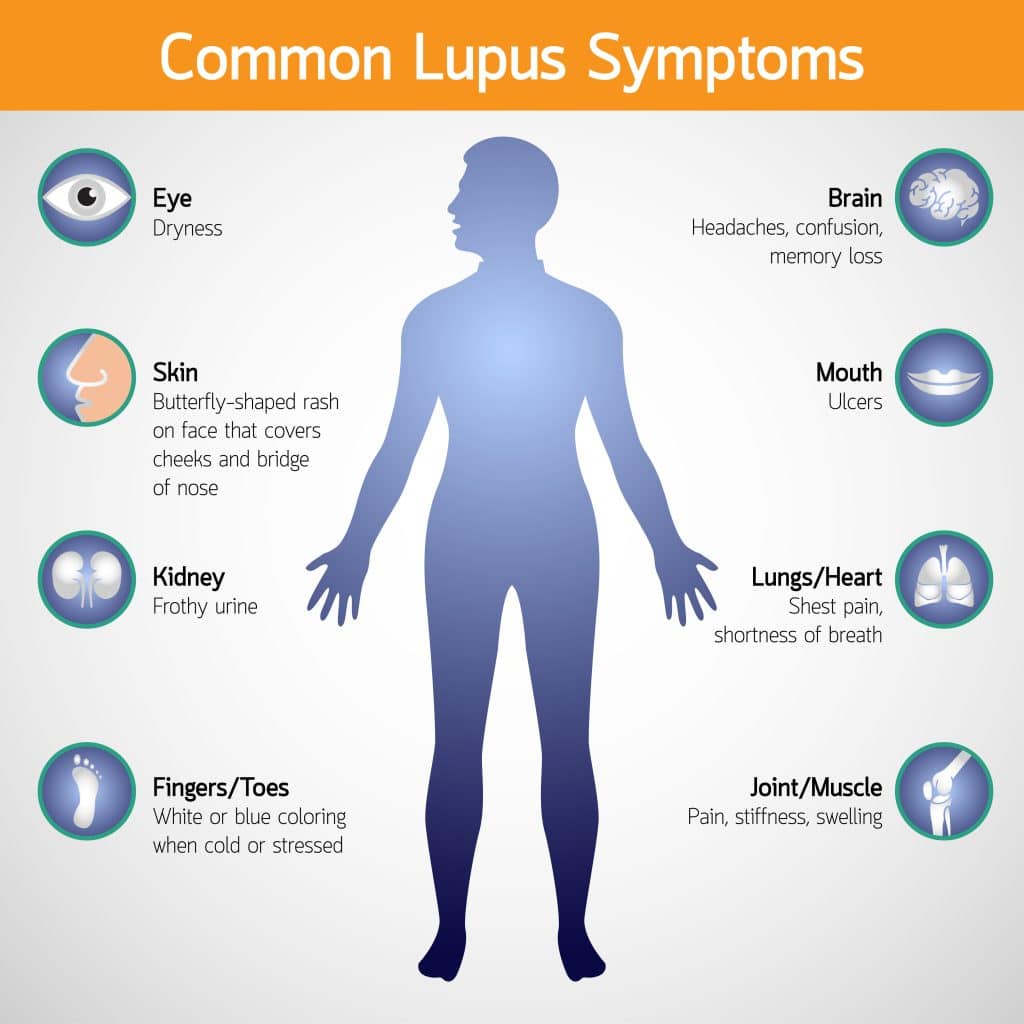
The main symptom of lupus is a butterfly-shaped rash that appears on the face. Other symptoms may include fatigue, fever, joint pain and swelling, chest pain, hair loss, sensitivity to the sun, anemia, swollen glands or organs in the body, headaches, and depression.
In some cases, patients may experience seizures or have difficulty with memory. Some people may also experience a decreased ability to think and reason clearly as a result of lupus. In addition, some individuals may develop anemia, a decrease in red blood cells that can lead to fatigue and other health issues.
Lastly, the presence of skin lesions is another common symptom of lupus. The lesions can range in size and appear on different body parts such as the face, chest, back, arms, and legs.2
What Are The Risk Factors For Developing Lupus?
The risk factors for developing lupus include being female. Lupus is more common in women than men, typically occurring between the ages of 15 and 45.
Oral contraceptive use has been linked with developing lupus.
Lupus also has a genetic component. Having a family member who has had lupus increases your risk of developing the disease.
Infection with the Epstein-Barr virus is linked with developing lupus.
Exposure to sunlight or ultraviolet light can result in lupus symptoms. People with lupus are more sensitive to sunlight and may develop a rash in response to exposure.
Certain medications, such as antimalarial drugs and certain antibiotics, have been linked to an increased risk of lupus.
Smoking cigarettes can increase the risk of developing lupus.
Stress has been linked to a worsening of lupus symptoms, which can lead to flare-ups.
Low levels of vitamin D and iron in the body have also been linked to an increased risk of developing lupus.
Pregnancy is another risk factor for lupus, as some women experience more frequent and severe flare-ups during this period.
Exposure to certain toxins, including air pollution, heavy metals, pesticides used in farming, and silica dust present in manufacturing may increase an individual’s risk of developing lupus.1
Difference Between Lupus And Systemic Lupus Erythematosus (SLE)
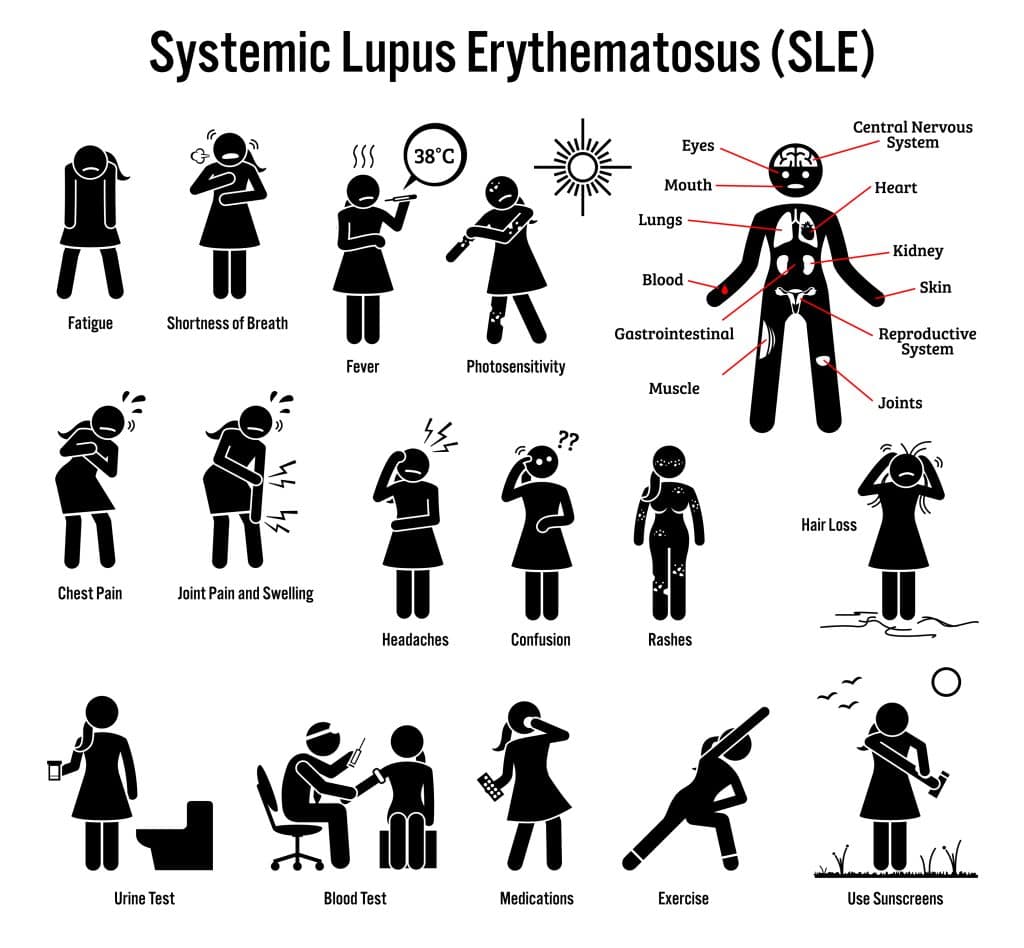
Systemic lupus erythematosus (SLE) is an autoimmune disease that can affect multiple parts of the body. It is characterized by inflammation, tissue destruction, and organ damage caused by the immune system attacking its own tissues.
Common symptoms of SLE include joint pain and swelling, skin rashes, fatigue, fever, and mouth ulcers. SLE is more common in women of childbearing age and it is thought to be triggered by environmental factors such as infections, drugs, hormones, or sunlight.
On the other hand, lupus is a general term that can refer to several autoimmune diseases, including SLE. While lupus can refer to a number of autoimmune diseases, SLE is the most common and best-known form of this condition.3
What Causes Lupus – Reducing The Risks – Sufficient Vitamin D Intake
Since sun exposure may not be possible for individuals suffering from lupus, as it exacerbates the condition, having an adequate amount of vitamin D in the body may help improve lupus.
Vitamin D is essential for the immune system, and research has shown that those with lower levels of vitamin D are more likely to develop lupus. While there is no definitive evidence to suggest taking a daily dose of vitamin D can prevent lupus, it is important to ensure your body has an adequate amount of this nutrient, especially when avoiding sunshine.
Eating foods that are naturally rich in vitamin D like fatty fish and mushrooms can help meet the daily recommendations. Additionally, consider supplementing with a vitamin D tablet or taking a multivitamin that includes vitamin D.
Taking a vitamin D supplement has been shown to reduce the risk of developing autoimmune conditions by 22%.4
What Causes Lupus – Silica Dust
The most common environmental factor associated with developing lupus is exposure to silica dust. Silica is a mineral found in many substances and materials, such as sand, soil, concrete, bricks, and quartz crystals. When these materials are crushed or disturbed, they release tiny particles of silica dust into the air that can be inhaled. The silica dust can then be absorbed by the lungs and cause inflammation, which may contribute to lupus flare-ups. Typically, only people who work in the manufacturing industry that are exposed to silica dust are affected.5 6
What Causes Lupus – Benzene Or Solvents
Benzene is a colorless, sweet-smelling chemical found in gasoline and other petroleum products. It can also be released into the air from burning coal, oil, or tobacco. Prolonged exposure to high levels of benzene can cause serious health problems such as leukemia, lymphoma, and immune system disorders including lupus.
Solvents are chemicals used to dissolve other substances, and some solvents have been linked to lupus. These include certain organic solvents such as trichloroethylene (TCE), perchloroethylene (PCE), and tetrachloroethylene (PCE).7
It is important to remember that even lower levels of these toxins from gasoline stations or other sources can pose a health risk over time, so avoiding exposure is key.
What Causes Lupus – Air Pollution
Air pollution is increasingly associated with the development and progression of lupus. Recent studies have suggested that exposure to air pollutants, such as nitrogen dioxide (NO2) and fine particulate matter, can increase an individual’s risk of developing lupus or experiencing more severe symptoms.
Studies have shown that higher levels of air pollution could potentially lead to an increased risk for lupus due to the body’s immune system being weakened as a result of exposure to toxins and other elements found in polluted air. In addition, studies suggest that air pollutants can cause systemic inflammation, which is a characteristic symptom of lupus.
Moreover, researchers believe that air pollution can lead to oxidative stress by releasing toxins and heavy metals into the bloodstream, which could potentially cause further damage to those with lupus. Oxidative stress is a condition where there is an imbalance between the production of reactive oxygen species (ROS) and antioxidant capacity in cells, and it has been linked to numerous illnesses, including lupus.6

What Causes Lupus – Pesticides
There is evidence that certain pesticides can contribute to the development of lupus. These include organochlorine and organophosphate insecticides. It’s thought that these chemicals are able to disrupt the body’s immune system and trigger an autoimmune response leading to lupus.8
What Causes Lupus – BPA
Bisphenol A (BPA) is a chemical found in many plastic products. BPA has been linked to an increased risk of lupus and other autoimmune diseases. BPA is an endocrine disruptor. This means it can mimic the effect of estrogen in the body and can affect hormone levels in the body. High exposure to BPA has been linked to an increased risk of lupus, due to its effects on the immune system.9
Research has also suggested a link between BPA and lupus nephritis, a type of kidney inflammation caused by lupus.10
BPA is also linked with weight loss resistance.15
What Causes Lupus – Heavy Metals
Studies have found that exposure to heavy metals is an underlying factor in developing lupus. Specifically, the heavy metals lead, cadmium, uranium, and mercury are linked with developing lupus.911
Mercury has been linked to many autoimmune disorders, including lupus. This means that anyone exposed to high levels of mercury, either through work or other activities, should take steps to protect themselves and be aware of the risks associated with prolonged exposure.12
Not surprisingly, dental workers are disproportionately affected by lupus, due to occupational exposure to mercury used in dental fillings.13

What Causes Lupus – The Connection Between Genetics And Toxins
Being genetically predisposed to developing lupus doesn’t mean you will definitely get this autoimmune condition. However, certain toxins like heavy metals, BPA, and many more impact genetic expression, which can lead to lupus.14 15
If the body has to use resources to deal with the side effects of toxicity, it doesn’t have enough resources to optimize epigenetic expression. Specifically, the body has to expend methyl groups to tame toxicity. Without enough methyl groups available to facilitate desirable epigenetic expression, a less-than-ideal version of our DNA is expressed.16 In this case, the phenotype for lupus and other autoimmune conditions is displayed.
The only way to deal with lupus and other autoimmune conditions is to remove the source of toxicity that is inhibiting ideal epigenetic expression. If we can remove toxins from our body, downregulate inflammation, and improve epigenetic expression, we can put an end to lupus.
Read more about how to stop inflammation and other autoimmune conditions.
References
1 Branch, N. S. C. a. O. (2022, March 7). The Future Directions of Lupus Research. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/about/future-directions-lupus-research
2 Lupus symptoms | Lupus Foundation of America. (2023). Lupus Foundation of America. https://www.lupus.org/resources/common-symptoms-of-lupus
3 Johns Hopkins Lupus Center. (2019, March 27). Types of Lupus : Johns Hopkins Lupus Center. https://www.hopkinslupus.org/lupus-info/types-lupus/
4 Bridger, H. (2022, January 27). Vitamin D reduced rate of autoimmune diseases by 22%. Harvard Gazette. https://news.harvard.edu/gazette/story/2022/01/vitamin-d-reduced-rate-of-autoimmune-diseases-by-22/
5 Finckh, A., Cooper, G. S., Chibnik, L. B., Costenbader, K. H., Watts, J., Pankey, H., Fraser, P. A., & Karlson, E. W. (2006). Occupational silica and solvent exposures and risk of systemic lupus erythematosus in urban women. Arthritis and rheumatism, 54(11), 3648–3654. https://doi.org/10.1002/art.22210
6 Cooper, G. S., Wither, J., Bernatsky, S., Claudio, J. O., Clarke, A., Rioux, J. D., CaNIOS GenES Investigators, & Fortin, P. R. (2010). Occupational and environmental exposures and risk of systemic lupus erythematosus: silica, sunlight, solvents. Rheumatology (Oxford, England), 49(11), 2172–2180. https://doi.org/10.1093/rheumatology/keq214
7 Blaskievicz, P. H., Silva, A. M. C., Fernandes, V., Junior, O. B. P., Shimoya-Bittencourt, W., Ferreira, S. M. B., & da Silva, C. A. L. (2020). Atmospheric Pollution Exposure Increases Disease Activity of Systemic Lupus Erythematosus. International journal of environmental research and public health, 17(6), 1984. https://doi.org/10.3390/ijerph17061984
8 Williams, J. N., Chang, S. C., Sinnette, C., Malspeis, S., Parks, C. G., Karlson, E. W., Fraser, P., & Costenbader, K. (2018). Pesticide exposure and risk of systemic lupus erythematosus in an urban population of predominantly African-American women. Lupus, 27(13), 2129–2134. https://doi.org/10.1177/0961203318805844
9 University of Cincinnati Academic Health Center. (2017, November 16). Environmental factors may trigger lupus onset, progression. ScienceDaily. Retrieved March 7, 2023 from www.sciencedaily.com/releases/2017/11/171116142056.htm
10 Dong, Y., Zhang, Z., Liu, H., Jia, L., Qin, M., & Wang, X. (2020). Exacerbating lupus nephritis following BPA exposure is associated with abnormal autophagy in MRL/lpr mice. American journal of translational research, 12(2), 649–659.
11 Barbhaiya, M., & Costenbader, K. H. (2016). Environmental exposures and the development of systemic lupus erythematosus. Current opinion in rheumatology, 28(5), 497–505. https://doi.org/10.1097/BOR.0000000000000318
12 Motts, J. A., Shirley, D. L., Silbergeld, E. K., & Nyland, J. F. (2014). Novel biomarkers of mercury-induced autoimmune dysfunction: a cross-sectional study in Amazonian Brazil. Environmental research, 132, 12–18. https://doi.org/10.1016/j.envres.2014.03.024
13 Bjørklund, G, Hilt, B, Dadar, M, Lindh, U, Aaseth, J. Neurotoxic effects of mercury exposure in dental personnel. Basic Clin Pharmacol Toxicol. 2019; 124: 568– 574. https://doi.org/10.1111/bcpt.13199
14 Khan, F., Momtaz, S., & Abdollahi, M. (2019). The relationship between mercury exposure and epigenetic alterations regarding human health, risk assessment and diagnostic strategies. Journal of trace elements in medicine and biology : organ of the Society for Minerals and Trace Elements (GMS), 52, 37–47. https://doi.org/10.1016/j.jtemb.2018.11.006
15 Neuroepic. (2022, June). BPA: Not A-gouti Thing for You –. https://neuroepic.mcdb.lsa.umich.edu/wp/14-bpa-not-a-gouti-thing-for-you/
16 Phillips, T. (2008) The role of methylation in gene expression. Nature Education 1(1):116