Gut Microbiome And Autoimmune Disease – Fixing The Microbiome
The link between the gut microbiome and autoimmune disease continues to get stronger as more research comes in. Autoimmune disease affects millions of people worldwide and the mainstream approach to dealing with these conditions involves treating the symptoms of these diseases rather than targetting the core cause. Here we’ll discuss what gut microbiome is, how it affects autoimmune disease, which autoimmune diseases are associated with it, and potential treatments through diet and supplements for managing autoimmunity.
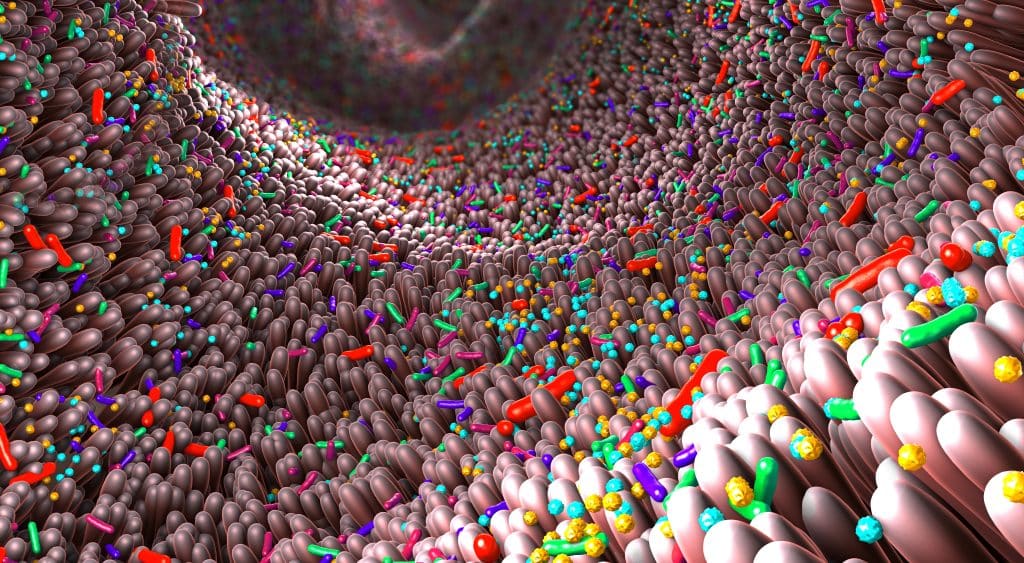
What Is the Gut Microbiome?
The gut microbiome, or microbiota, refers to the trillions of bacteria that live in our digestive tract or gastrointestinal (GI) tract. The diversity and composition of these microbes play an important role in our health by aiding digestion, synthesizing nutrients, and regulating the immune system. This complex microbial ecosystem is ever-changing and can be affected by our diet, lifestyle, and environment.1
Overview Of Autoimmune Disease
Autoimmune disease occurs when the body’s immune system mistakenly attacks its own cells. This leads to inflammation and tissue damage that manifests in various symptoms depending on the type of autoimmune disorder. Common ones include rheumatoid arthritis, multiple sclerosis, inflammatory bowel disease, celiac disease, and psoriasis.
Read more about what causes autoimmune diseases.
Interaction Between The Microorganisms And The Immune System
The interaction between the microorganisms and the immune system can be complex, and it can involve different signals. The immune system is responsible for two main roles, fighting off pathogens and maintaining homeostasis. Microorganisms help the body in various ways such as providing nutrients to certain organs or breaking down molecules that cannot be broken down by the human body on its own. In addition, they also act as a barrier against infection from other pathogens.2
As a result, the immune system must be able to distinguish between beneficial and harmful microorganisms in order to maintain balance. The immune system does this by releasing cytokines, which are molecules that signal different cells of the immune system to respond in certain ways. For example, they can signal macrophages to kill bacteria or phagocytes to engulf and digest foreign particles. They can also stimulate the production of antibodies to fight infection and activate T-cells to attack abnormal cells in the body. These interactions between the immune system and microorganisms enable the body to maintain homeostasis, as well as protect it from infection and disease.
The immune system is also responsible for recognizing foreign substances that enter the body, such as allergens. Allergens, which are small proteins or particles that can cause an allergic reaction when they enter the body, are usually harmless for most individuals. However, in some people with allergies, their immune system will respond to these allergens as if they were a pathogen and launch an attack against them. This immune response leads to symptoms such as itching and sneezing.3
The immune system’s interaction with microorganisms is essential for maintaining the body’s health and well-being. Without these interactions, the body would be unable to fight off infections or recognize potential harm.

How Does The Gut Microbiome Affect Autoimmune Disease?
The gut microbiome has a complex relationship with the immune system. It interacts with both beneficial and harmful microorganisms, which can lead to dysbiosis if the balance is disrupted. Dysbiosis is an imbalance in the microbial ecosystem, resulting from factors like antibiotic use, poor diet, stress, and environmental toxins. This condition can cause inflammation and potentially trigger autoimmune diseases.4
Role Of Dysbiosis In Inflammation And Autoimmunity
Dysbiosis has been proposed to play an important role in the development of inflammation and autoimmunity. It is now established that dysregulation of the gut microbiome, through either reduced microbial diversity or alterations in bacterial composition, can lead to a state of chronic inflammation within the body. This is thought to occur due to increased levels of pro-inflammatory cytokines, which stimulate the activation of immune cells and contribute to the development of autoimmune-related pathology.
Dysbiosis has also been linked to a decrease in regulatory T cells, which are important for maintaining immune tolerance and preventing autoimmunity. In addition, some bacteria may produce toxins that can damage host tissues and trigger an immune response that can ultimately lead to autoimmunity. Finally, certain bacteria may secrete substances that can mimic the structure of host proteins and lead to autoimmunity via molecular mimicry. Together, these mechanisms suggest that dysbiosis is an important factor in the development of inflammation and autoimmunity.5
Microbiome Dysbiosis – Antibiotic Use
The use of antibiotics has long been associated with the disruption and imbalance of the human microbiome. Antibiotics target bacteria, both beneficial and pathogenic, indiscriminately, leading to a disturbance in the microbial balance. This can lead to an increase in pathogenic bacteria that cause disease or infection, called dysbiosis. The effects of dysbiosis depend on the body site, the type of antibiotic used, and the duration of treatment.6
Microbiome Dysbiosis – Heavy Metals
Heavy metal toxicity has been linked to microbiome dysbiosis, leading to significant changes in the composition and function of the microbiota. Heavy metals such as lead, cadmium, mercury, and arsenic are known to disrupt microbial communities and decrease their diversity.
For instance, lead has been shown to interfere with the production of essential enzymes involved in metabolic processes, while mercury has been shown to reduce the number of beneficial bacteria and increase the levels of pathogenic species. In addition, exposure to these heavy metals can cause changes in the gut microbial populations that can result in inflammation and other conditions such as irritable bowel syndrome.
Read more about irritable bowel syndrome.
Furthermore, long-term exposure to these toxic substances leads to an altered composition of the microbiome that is associated with the development of various diseases. Therefore, it is important to understand how these heavy metals interact with the microbiome in order to design effective strategies that can mitigate their effects and promote healthy microbial communities.7 8

Microbiome Dysbiosis – Glyphosate
Glyphosate is a commonly used herbicide that has been linked to microbiome dysbiosis. Research has shown that glyphosate can disrupt the normal balance of bacteria in the gut, leading to diseases such as inflammatory bowel disease (IBD). In addition, glyphosate has been found to alter microbial metabolism and reduce beneficial bacterial species.
Read more about inflammatory bowel disease.
This disruption of the normal microbial population can lead to an overgrowth of pathogenic bacteria, increased inflammation, and decreased immune system function. Furthermore, research suggests that glyphosate-based herbicides can also contribute to gastrointestinal distress such as abdominal cramping and bloating.9 10
Microbiome Dysbiosis – Air Pollution
Air pollution is known to have an impact on the human microbiome. Studies show air pollution can disrupt the balance of our microbiome. This disruption has been linked to a variety of health effects such as respiratory tract infections, asthma, allergies, and even cardiovascular diseases. Additionally, research suggests that air pollution may disrupt the immune system and decrease its ability to fight off diseases.
The link between air pollution and microbiome dysbiosis is related to pollutants such as particulate matter (PM), nitrogen dioxide (NO2), sulfur dioxide (SO2), carbon monoxide (CO), and ozone (O3). These pollutants are known to damage cells and tissues, leading to increased inflammation. This inflammation can affect the composition of the microbiome by reducing beneficial bacteria and allowing harmful ones to flourish.11 12
Gut Microbiome And Autoimmune Disease
Studies have found that many common autoimmune diseases may be associated with changes in the gut microbiome. These include rheumatoid arthritis, multiple sclerosis, inflammatory bowel disease (IBD), celiac disease, psoriasis, and Sjogren’s syndrome.13
The Gut Microbiome And Autoimmune Disease
Recent research has shed light on the role of the gut microbiome in autoimmune disease. One study suggests that certain microorganisms can contribute to inflammation and autoimmunity by disrupting immune system homeostasis. Additionally, the hygiene hypothesis proposes that an overly-sanitized environment decreases microbial diversity in our GI tract, which may lead to increased rates of autoimmune disorders.14
Diet interventions have also been shown to play a role in managing autoimmunity. Eliminating refined sugars, processed foods, and inflammatory foods like dairy or gluten may help reduce symptoms. Eating a clean diet, like my Cellular Healing Diet is the first step to improving the microbiome.
Read more about my Cellular Healing Diet.
Additionally, incorporating probiotics into the diet can support a healthy microbial balance in the gut. Probiotics are live microorganisms found in fermented foods like yogurt and kimchi.15
Finally, fecal microbial transplantation (FMT) is an emerging treatment for autoimmune disease due to its ability to restore dysbiosis in the gut microbiome. FMT has been used successfully to treat many autoimmune conditions including Crohn’s disease, ulcerative colitis, and multiple sclerosis.16
Gut Microbiome And Autoimmune Disease
The link between the gut microbiome and autoimmune disease is clear. This is because the gut microbiome plays an important role in regulating the immune system. Research is beginning to uncover new treatments for autoimmunity that involve diet interventions and supplementations with probiotics and fecal microbial transplantation therapy. However, the connection between the gut microbiome and autoimmune disease is only one piece of the puzzle, as there are other factors that contribute to the development of autoimmune conditions.
Read more about what causes autoimmune conditions.
References
1 Thursby E, Juge N. Introduction to the human gut microbiota. Biochem J. 2017 May 16;474(11):1823-1836. doi: 10.1042/BCJ20160510. PMID: 28512250; PMCID: PMC5433529.
2 Hooper LV, Macpherson AJ. Immune adaptations that maintain homeostasis with the intestinal microbiota. Nat Rev Immunol. 2010 Mar;10(3):159-69. doi: 10.1038/nri2710. PMID: 20182457.
3 Wiertsema SP, van Bergenhenegouwen J, Garssen J, Knippels LMJ. The Interplay between the Gut Microbiome and the Immune System in the Context of Infectious Diseases throughout Life and the Role of Nutrition in Optimizing Treatment Strategies. Nutrients. 2021 Mar 9;13(3):886. doi: 10.3390/nu13030886. PMID: 33803407; PMCID: PMC8001875.
4 Kelly, J., Kennedy, P., Cryan, J., Dinan, T., Clarke, G. (2015). Breaking down the barriers: The gut microbiome, intestinal permeability and stress-related psychiatric disorders. Frontiers in Cellular Neuroscience 9(2), 1-14. doi:10.3389/fncel.2015.00050
5 Kang, D., Adams, J. B., Coleman, D. M., & Liu, Y. (2016). Dysbiosis of the gut microbiota in disease. Microbiology Specturm 4(3), 1-30. doi:10.1128/microbiolspec.DBIO-0027-2015
6 Ramirez J, Guarner F, Bustos Fernandez L, Maruy A, Sdepanian VL, Cohen H. Antibiotics as Major Disruptors of Gut Microbiota. Front Cell Infect Microbiol. 2020 Nov 24;10:572912. doi: 10.3389/fcimb.2020.572912. PMID: 33330122; PMCID: PMC7732679.
7 Bist P, Choudhary S. Impact of Heavy Metal Toxicity on the Gut Microbiota and Its Relationship with Metabolites and Future Probiotics Strategy: a Review. Biol Trace Elem Res. 2022 Dec;200(12):5328-5350. doi: 10.1007/s12011-021-03092-4. Epub 2022 Jan 7. PMID: 34994948.
8 Assefa S, Köhler G. Intestinal Microbiome and Metal Toxicity. Curr Opin Toxicol. 2020 Feb;19:21-27. doi: 10.1016/j.cotox.2019.09.009. Epub 2019 Sep 30. PMID: 32864518; PMCID: PMC7450720.
9 Rueda-Ruzafa L, Cruz F, Roman P, Cardona D. Gut microbiota and neurological effects of glyphosate. Neurotoxicology. 2019 Dec;75:1-8. doi: 10.1016/j.neuro.2019.08.006. Epub 2019 Aug 20. PMID: 31442459.
10 Aitbali Y, Ba-M’hamed S, Elhidar N, Nafis A, Soraa N, Bennis M. Glyphosate based- herbicide exposure affects gut microbiota, anxiety and depression-like behaviors in mice. Neurotoxicol Teratol. 2018 May-Jun;67:44-49. doi: 10.1016/j.ntt.2018.04.002. Epub 2018 Apr 7. PMID: 29635013.
11 Liou A P Y, Bousvaros A., Bäckhed F., & Powrie F. (2013). Microbiota modulation of inflammation and autoimmune diseases: Mechanisms and therapeutic potentials. Immunology 140(1), 15–22. Doi: 10.1111/imm.12086
12 Moelling K, Broecker F. Air Microbiome and Pollution: Composition and Potential Effects on Human Health, Including SARS Coronavirus Infection. J Environ Public Health. 2020 May 28;2020:1646943. doi: 10.1155/2020/1646943. PMID: 32565838; PMCID: PMC7256708.
13 Xu Q, Ni JJ, Han BX, Yan SS, Wei XT, Feng GJ, Zhang H, Zhang L, Li B, Pei YF. Causal Relationship Between Gut Microbiota and Autoimmune Diseases: A Two-Sample Mendelian Randomization Study. Front Immunol. 2022 Jan 24;12:746998. doi: 10.3389/fimmu.2021.746998. PMID: 35140703; PMCID: PMC8819003.
14 Al Bander Z, Nitert MD, Mousa A, Naderpoor N. The Gut Microbiota and Inflammation: An Overview. Int J Environ Res Public Health. 2020 Oct 19;17(20):7618. doi: 10.3390/ijerph17207618. PMID: 33086688; PMCID: PMC7589951.
15 Wieërs G, Belkhir L, Enaud R, Leclercq S, Philippart de Foy JM, Dequenne I, de Timary P, Cani PD. How Probiotics Affect the Microbiota. Front Cell Infect Microbiol. 2020 Jan 15;9:454. doi: 10.3389/fcimb.2019.00454. PMID: 32010640; PMCID: PMC6974441.
16 Yin, Y., Wang, T. H., & Tan, C. S. (2020). Fecal microbiota transplantation for autoimmune diseases: A systematic review and meta-analysis of randomized controlled trials. Journal of Gastroenterology and Hepatology 35(4), 748–758. doi:10.1111/jgh.14919




