The Connection Between A Deficiency Of Vitamin D And Autoimmune Conditions
Recent research suggests that there is a strong link between a deficiency of vitamin D and autoimmune conditions. Studies indicate that vitamin D can reduce chronic inflammation, which is the underlying cause of autoimmune diseases.
What Is Vitamin D?
Vitamin D is a fat-soluble vitamin that helps your body absorb calcium and phosphorus. It is important for proper growth, development, immune system health, and strong bones.
Vitamin D has been shown to have various immunomodulatory, anti-inflammatory, antioxidant, and anti-fibrotic effects. This is important in the context of autoimmune diseases, which are characterized by abnormal activation of the immune system that causes it to attack its own harmless antigens.1
How Do We Get Vitamin D?
Vitamin D is naturally produced by the body when exposed to sunlight and can also be obtained from food sources such as fatty fish, egg yolks, mushrooms, fortified foods, and supplements. To get the most out of vitamin D, receive regular sun exposure, even as little as 15 minutes a day. Additionally, make sure your diet includes adequate amounts of vitamin D, ideally in the form of food.
Vitamin D And Autoimmune Conditions
Vitamin D helps to regulate the body’s immune system, which is key in preventing or reducing autoimmune disease flare-ups. It does this by activating certain cells in the immune system, such as T cells and B cells, which help to eliminate foreign substances that could cause inflammation or an autoimmune response.
Vitamin D helps regulate the production of cytokines, which are small proteins released by various cells that help regulate the body’s response to infection and inflammation. Research suggests that high levels of certain cytokines, such as interleukin-17 (IL-17) can contribute to autoimmune diseases.2
Even though excessive vitamin D supplementation can create imbalances in other important vitamins, many studies show that supplementing with vitamin D improves symptoms of autoimmune conditions. For example, a recent systematic review found that vitamin D supplementation can reduce inflammation and pain in patients with rheumatoid arthritis. Taking a vitamin D supplement (2,000 IU per day) has been demonstrated to decrease the likelihood of developing autoimmune disorders by 22%.3

Vitamin D And Tuberculosis
Vitamin D has been used as a treatment for tuberculosis since before the introduction of antibiotics. In the past, patients suffering from tuberculosis were confined to sanatoriums and exposed to sunlight in order to kill the bacteria. Cod liver oil, which is an excellent source of vitamin D, was also prescribed as an additional means of protecting against tuberculosis and other infections.4
Vitamin D And Immunity
In a study on 800 military recruits in Finland, those with lower levels of vitamin D were found to miss significantly more days from active duty due to upper respiratory infections than those whose levels of vitamin D were higher.5
There have also been a number of other cross-sectional studies exploring the relationship between vitamin D levels and the rate of influenza, bacterial vaginosis, and HIV.6 7 8 In fact, sufficient vitamin D levels are associated with a 42% reduction in cases of influenza.9 All of these studies have found a link between lower vitamin D levels and increased rates of infection.
Vitamin D And Autoimmune Conditions – A Look At The Research
There is a strong correlation between lower levels of vitamin D and the development of several autoimmune diseases such as lupus, thyrotoxicosis, multiple sclerosis (MS), iridocyclitis, Crohn’s disease, ulcerative colitis, psoriasis vulgaris, rheumatoid arthritis (RA), and polymyalgia rheumatica.1
Vitamin D And Autoimmune Conditions – Multiple Sclerosis (MS)
Recent research suggests that people with low vitamin D levels are at an increased risk of developing multiple sclerosis (MS). A study on 7 million Army and Navy personnel has found a correlation between lower vitamin D levels and greater severity of MS symptoms.10
Vitamin D is a key component of T cell homeostasis in patients with multiple sclerosis. T cell homeostasis helps ensure that the body’s immune system is able to efficiently detect and respond to threats. To maintain homeostasis, the T cells must be able to recognize self-antigens and ignore non-self antigens. Failure of this process can result in autoimmunity or immunological disorders like MS.11
Read more about what causes Mulitple Sclerosis.
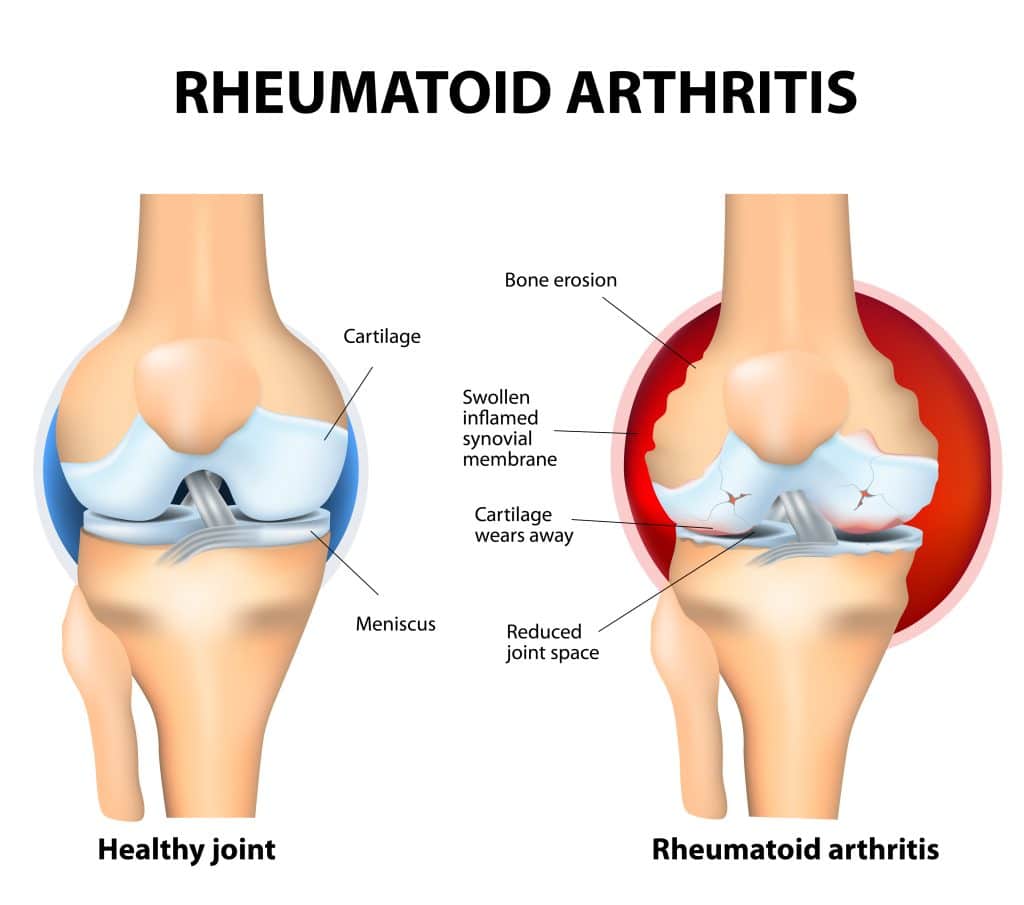
Vitamin D And Autoimmune Conditions – Rheumatoid Arthritis (RA)
Studies have shown that people with RA tend to have lower levels of vitamin D in their blood than those without the condition. Low vitamin D levels can make it harder to fight off inflammation, which is a key factor in RA. Supplementing with vitamin D has been found to reduce the severity of RA symptoms and slow the progress of the disease.13
Read more about what causes RA.
Vitamin D And Autoimmune Conditions – Lupus
Vitamin D supplementation has been shown to reduce symptoms of lupus. One study found that after 3 months of supplementation with high doses of vitamin D3, lupus patients experienced a significant reduction in fatigue and joint pain. Other studies have shown that supplementation can reduce the levels of inflammatory markers and improve the quality of life for people with lupus.14
Read more about what causes lupus.
Vitamin D And Autoimmune Conditions – Thyrotoxicosis
Thyrotoxicosis is an autoimmune condition that occurs when the body produces too much thyroid hormone. Studies have suggested that low levels of vitamin D may be a risk factor for this condition. Taking a supplement containing both vitamin D and calcium may reduce the risk of developing thyrotoxicosis.15
Read more about thyroid disorders.
Vitamin D And Autoimmune Conditions – Iridocyclitis
Iridocyclitis, an autoimmune condition of the eye, has been linked to vitamin D levels. Research suggests that having a low level of vitamin D may increase your risk of getting iridocyclitis.1
Vitamin D And Autoimmune Conditions – Crohn’s Disease
Crohn’s Disease is an autoimmune disorder that affects the digestive system. It can cause painful and uncomfortable symptoms such as diarrhea, abdominal pain, fatigue, and weight loss. Vitamin D has been found to be beneficial in reducing inflammation associated with Crohn’s Disease and may also play a role in preventing flare-ups of the condition. Studies have found that lower levels of vitamin D in the blood are associated with increased severity of Crohn’s disease symptoms.16

Vitamin D And Autoimmune Conditions – Ulcerative Colitis
Recent research suggests that vitamin D could play an important role in the treatment of ulcerative colitis (UC), an autoimmune digestive disorder. In people with UC, their own immune system mistakenly attacks their healthy intestinal tissue and causes inflammation.
This can result in abdominal pain, frequent diarrhea, weight loss, and fatigue. Studies have shown that supplementing with vitamin D can help reduce inflammation and associated symptoms of UC. Additionally, low levels of vitamin D have been linked to a higher risk of developing ulcerative colitis. Therefore, it is important for individuals with this condition to ensure they are receiving adequate amounts of vitamin D, ideally through their diet or sun exposure.17
Vitamin D And Autoimmune Conditions – Psoriasis Vulgaris
Low vitamin D levels can lead to an overactive immune system, which can contribute to the development of psoriasis vulgaris. Studies have shown that supplementing with vitamin D3 or taking a calcium-vitamin D supplement may be beneficial for those with psoriasis vulgaris. Vitamin D3 specifically has been found to reduce symptoms of psoriasis vulgaris and improve the skin’s appearance. Vitamin D can also help prevent flare-ups of psoriasis vulgaris, as well as aid in wound healing.18
Vitamin D And Autoimmune Conditions – Polymyalgia Rheumatica
Polymyalgia rheumatica (PMR) is an autoimmune disorder that is characterized by inflammation of the muscles and joints. Recent evidence suggests that vitamin D deficiency may be a contributing factor to this condition. Low levels of vitamin D can lead to decreased immune function which can make individuals more susceptible to autoimmune diseases such as PMR.
Studies have shown that vitamin D supplementation can reduce the symptoms of PMR, improve joint mobility, and even reduce inflammation in some cases. Additionally, vitamin D may also help to decrease the number of medications required for the effective treatment of PMR.19
How To Get Enough Vitamin D
In addition to foods that contain high levels of vitamin D, increasing your exposure to natural sunlight is an effective way to boost vitamin D levels. Just 15 minutes of exposure to sunlight can increase your body’s vitamin D levels significantly. Therefore, it is important to get some sun exposure daily, even during the winter months.
Supplementing with vitamin D comes with some risks, especially if consumed excessively. For starters, high doses of vitamin D increase the amount of calcium in the blood that in turn results in blood vessel calcification.20 Secondly, high doses of vitamin D are linked to a vitamin K deficiency.21 While many people consume vitamin D with vitamin K to prevent this issue, obtaining both vitamins from natural means is a better option.
Reduce The Progression Of Autoimmune Diseases With Vitamin D
The body requires adequate vitamin D to maintain a healthy immune system and regulate inflammation. A vitamin D deficiency is especially pronounced in individuals with autoimmune diseases. The highest correlation between vitamin D and autoimmune conditions is noted in rheumatoid arthritis, multiple sclerosis, and lupus.
Read more about what causes autoimmune conditions.
References
1 Murdaca G, Tonacci A, Negrini S, Greco M, Borro M, Puppo F, Gangemi S. Emerging role of vitamin D in autoimmune diseases: An update on evidence and therapeutic implications. Autoimmun Rev. 2019 Sep;18(9):102350. doi: 10.1016/j.autrev.2019.102350. Epub 2019 Jul 16. PMID: 31323357.
2 Almerighi C, Sinistro A, Cavazza A, Ciaprini C, Rocchi G, Bergamini A. 1Alpha,25-dihydroxyvitamin D3 inhibits CD40L-induced pro-inflammatory and immunomodulatory activity in human monocytes. Cytokine. 2009 Mar;45(3):190-7. doi: 10.1016/j.cyto.2008.12.009. Epub 2009 Jan 30. PMID: 19186073.
3 Bridger, H. (2022, January 27). Vitamin D reduced rate of autoimmune diseases by 22%. Harvard Gazette. https://news.harvard.edu/gazette/story/2022/01/vitamin-d-reduced-rate-of-autoimmune-diseases-by-22/
4 Williams, C. J. B. (1849). 7.–On the Use and Administration of Cod-Liver Oil in Pulmonary Consumption. The Ohio Medical and Surgical Journal (1848-1878), 2(1), 50.
5 Laaksi I, et al. An association of serum vitamin D concentrations < 40 nmol/L with acute respiratory tract infection in young Finnish men. Am J Clin Nutr. 2007;86(3):714–7.
6 Cannell JJ, et al. Epidemic influenza and vitamin D. Epidemiol Infect. 2006;134(6):1129–40.
7 Bodnar LM, Krohn MA, Simhan HN. Maternal vitamin D deficiency is associated with bacterial vaginosis in the first trimester of pregnancy. J Nutr. 2009;139(6):1157–61.
8 Villamor E. A potential role for vitamin D on HIV infection? Nutr Rev. 2006;64(5 Pt 1):226–33.
9 Urashima M, et al. Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren. Am J Clin Nutr. 2010;91(5):1255–60.
10 Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA. 2006 Dec 20;296(23):2832-8. doi: 10.1001/jama.296.23.2832. PMID: 17179460.
11 Correale J, Ysrraelit MC, Gaitán MI. Immunomodulatory effects of Vitamin D in multiple sclerosis. Brain. 2009 May;132(Pt 5):1146-60. doi: 10.1093/brain/awp033. Epub 2009 Mar 24. PMID: 19321461.
13 Merlino LA, Curtis J, Mikuls TR, Cerhan JR, Criswell LA, Saag KG; Iowa Women’s Health Study. Vitamin D intake is inversely associated with rheumatoid arthritis: results from the Iowa Women’s Health Study. Arthritis Rheum. 2004 Jan;50(1):72-7. doi: 10.1002/art.11434. PMID: 14730601.
14 Kamen D, Aranow C. Vitamin D in systemic lupus erythematosus. Curr Opin Rheumatol. 2008 Sep;20(5):532-7. doi: 10.1097/BOR.0b013e32830a991b. PMID: 18698173.
15 Taheriniya, S., Arab, A., Hadi, A. et al. Vitamin D and thyroid disorders: a systematic review and Meta-analysis of observational studies. BMC Endocr Disord 21, 171 (2021). https://doi.org/10.1186/s12902-021-00831-5
16 White JH. Vitamin D deficiency and the pathogenesis of Crohn’s disease. J Steroid Biochem Mol Biol. 2018 Jan;175:23-28. doi: 10.1016/j.jsbmb.2016.12.015. Epub 2016 Dec 23. PMID: 28025175.
17 Wang H, He X, Liang S, Chen X. Role of vitamin D in ulcerative colitis: an update on basic research and therapeutic applications. Expert Rev Gastroenterol Hepatol. 2022 Mar;16(3):251-264. doi: 10.1080/17474124.2022.2048817. Epub 2022 Mar 8. PMID: 35236213.
18 Rucević I, Barisić-Drusko V, Glavas-Obrovac L, Stefanić M. Vitamin D endocrine system and psoriasis vulgaris–review of the literature. Acta Dermatovenerol Croat. 2009;17(3):187-92. PMID: 19818218.
19 Acharya S, Musa R. Polymyalgia Rheumatica. [Updated 2022 Jun 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537274/
20 Pérez-Barrios C, Hernández-Álvarez E, Blanco-Navarro I, Pérez-Sacristán B, Granado-Lorencio F. Prevalence of hypercalcemia related to hypervitaminosis D in clinical practice. Clin Nutr. 2016 Dec;35(6):1354-1358. doi: 10.1016/j.clnu.2016.02.017. Epub 2016 Mar 8. PMID: 26995293.
21 Masterjohn C. Vitamin D toxicity redefined: vitamin K and the molecular mechanism. Med Hypotheses. 2007;68(5):1026-34. doi: 10.1016/j.mehy.2006.09.051. Epub 2006 Dec 4. PMID: 17145139.




