What Causes Myasthenia Gravis – And How To Manage It
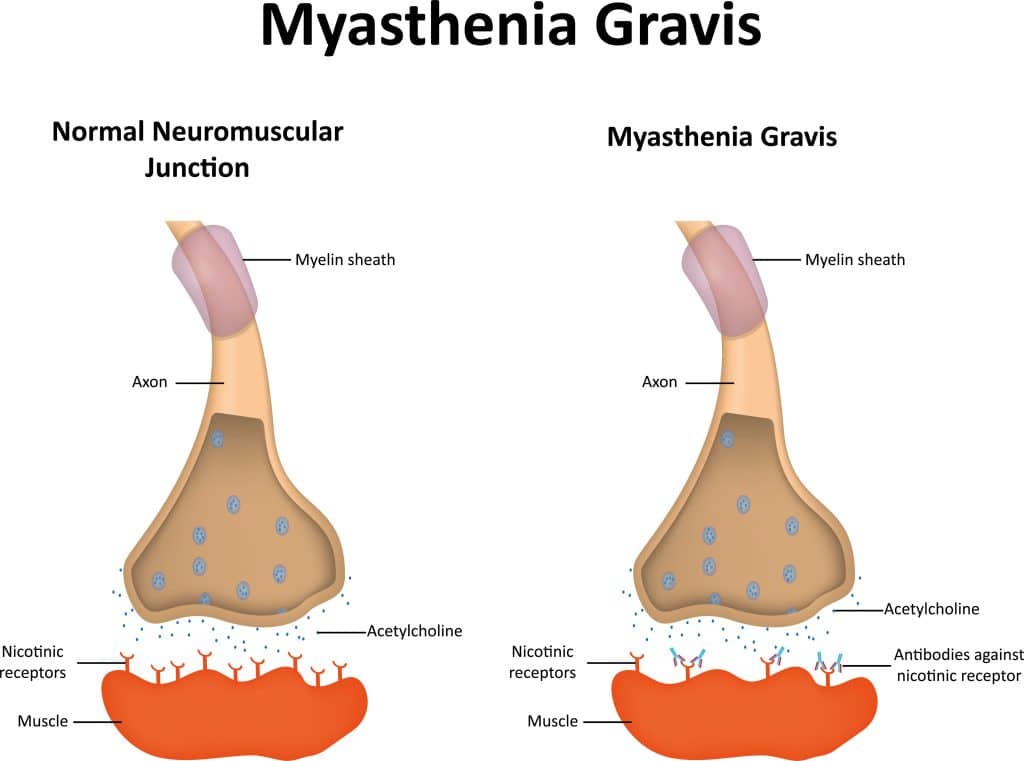
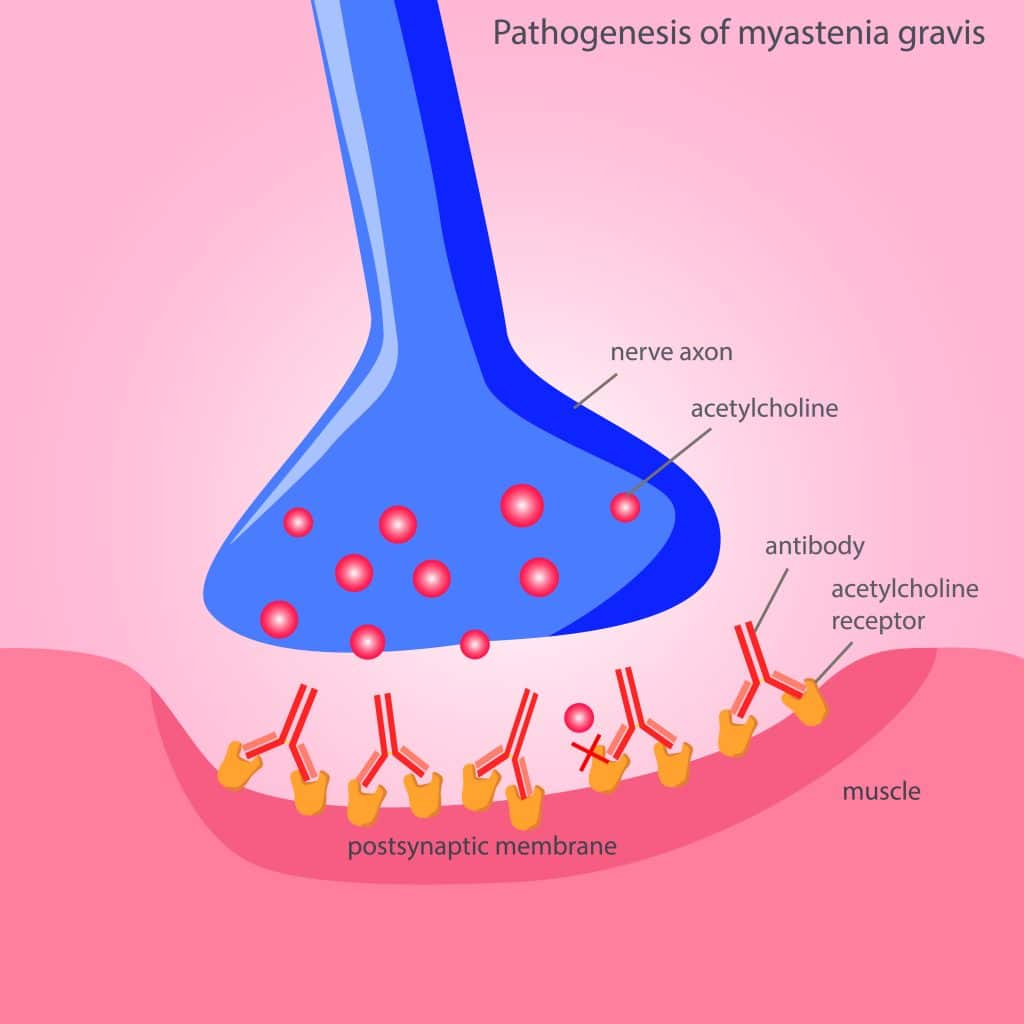
Exactly what causes myasthenia gravis (MG) is an abnormal immune system response in which the body’s own antibodies attack and damage receptors for acetylcholine, a neurotransmitter that helps control muscle movement. Myasthenia Gravis is an autoimmune disorder that affects the connection between the nerves and muscles. This leads to a severe weakening of muscle strength, leading to difficulty in speaking, eating, and even walking or standing.
The most common symptoms include drooping eyelids, blurred vision due to double vision, fatigue, and general weakness in arms and legs. In more serious cases, it can cause difficulty in swallowing food and breathing.
Myasthenia gravis has been linked to dysfunction of the thymus gland, which is located at the base of the neck behind the breastbone. The thymus gland plays an important role in our immune system as it produces T-cells that fight against infections and other foreign materials. In people with myasthenia gravis, the thymus gland may be overactive or underactive, leading to abnormal antibody production that attacks the body’s own muscle tissue.
It is unknown why this autoimmune reaction occurs in some individuals, but like other autoimmune conditions, it is related to genetics and environmental triggers. Treatment focuses on strengthening remaining muscles, suppressing the production of antibodies, and improving communication between nerves and muscles. Medications such as acetylcholinesterase inhibitors and immunosuppressants are often used to reduce muscle weakness and fatigue. In some cases, surgery may be needed to remove part of the thymus gland in order to reduce its activity. The procedure is called a thymectomy.1
What Is A Myasthenic Crisis?
A myasthenic crisis is a serious condition in which the symptoms of myasthenia gravis become suddenly and severely worse. Symptoms of a myasthenic crisis can include difficulty breathing or swallowing, drooping eyelids, slurred speech, and extreme fatigue.
Treatment for a myasthenic crisis usually involves hospitalization, medications to reduce muscle weakness and improve airway function, intravenous immunoglobulins (IVIg) to help restore nerve-muscle communication, and/or plasmapheresis (plasma exchange) to remove harmful antibodies. With prompt treatment, most people with a myasthenic crisis can make a full recovery.2
What Causes Myasthenia Gravis – 3-Legged Stool
Autoimmune conditions like Myasthenia Gravis have numerous factors that all play a role. This is what I call the 3-legged stool, as all three of these factors need to be in play for the progression of autoimmune conditions.
First, genetic factors and epigenetic factors play a role along with environmental factors and microbiome dysfunction. The key to managing or treating autoimmune conditions is to remove the environmental factors that are linked to these conditions, improve epigenetic expression, and restore microbiome health.
Read more about the factors that cause autoimmune conditions.
What Causes Myasthenia Gravis – Genetics
Genetic factors have been shown to play a role in myasthenia gravis. A mutated gene that disrupts neuromuscular transmission has been linked to some cases of myasthenia gravis. The mutation affects the structure of acetylcholine receptors on the surface of muscle cells, interfering with their ability to transmit signals from the nerves to the muscles. In cases where myasthenia gravis is inherited, it usually occurs in families and is caused by a mutation in one or both of two genes, called AChR (acetylcholine receptor) and MuSK (muscle-specific kinase). These mutations are passed down from one generation to the next.3 4
What Causes Myasthenia Gravis – Epigenetics
Myasthenia gravis is caused by a combination of genetic factors and environmental influences, such as epigenetics.
Epigenetics is the study of how experiences or environmental factors can influence gene expression, without changing the (DNA) sequence of a gene. In the case of myasthenia gravis, epigenetic changes may contribute to the development of autoantibodies against proteins in the muscle-nerve pathway.
Epigenetic changes can be caused by several external influences, such as diet and lifestyle choices, exposure to toxins, and the use of certain medications. While these influences may not directly cause myasthenia gravis, they can contribute to the development of this condition by altering how a person’s genes are expressed.
In addition to environmental factors, epigenetic changes can be passed down through generations. This means that even if a person does not have an identified genetic mutation or disease, they can still be at higher risk of developing myasthenia gravis if their parents or grandparents had the condition.5
What Causes Myasthenia Gravis – Viral Infections
Viral infections like hepatitis C, Epstein-Barr virus herpes simplex virus, West Nile Virus, Influenza A, and COVID-19 are all linked with Myasthenia Gravis.6
What Causes Myasthenia Gravis – Other Autoimmune Conditions
Myasthenia Gravis can be caused by other autoimmune conditions. These include Autoimmune Thyroiditis, Systemic Lupus Erythematosus (SLE), Sjogren’s Syndrome, and Rheumatoid Arthritis (RA). Each of these diseases causes the body to produce autoantibodies that attack its own healthy tissues.7
Myasthenia Gravis And Thyroid Disorders
People with thyroid conditions, specifically hyperthyroidism (an overactive thyroid) are at an increased risk for developing myasthenia gravis. In patients with hyperthyroidism, the immune system is overactive and produces antibodies that attack the nerve cells in the neuromuscular junction. This can lead to muscle weakness and fatigue. In addition, some studies suggest that hyperthyroidism may increase the risk of developing myasthenia gravis.8
Myasthenia Gravis And Graves’ Disease
Myasthenia gravis and Graves’ disease are two of the most common autoimmune disorders that affect the neuromuscular junction. Graves’ disease is an autoimmune disorder where the antibodies produced by the immune system attack the thyroid gland, causing it to produce too much thyroid hormone. Symptoms of Graves’ disease can include fatigue, weight loss, sweating, rapid heart rate, goiter, and bulging eyes.9
Read more about Graves’ Disease.
What Causes Myasthenia Gravis – Pesticides
Exposure to certain pesticides, such as organophosphates and carbamates, can interfere with the functioning of the neuromuscular junction in the body. This is because these types of chemicals affect how nerve signals interact with muscle fibers, leading to muscle weakness. Additionally, some studies have indicated that those who are exposed to a variety of different chemicals are at an increased risk of developing myasthenia gravis.10 11

What Causes Myasthenia Gravis – Iron Deficiency
Individuals with Myasthenia gravis were found to have an iron deficiency, which can weaken the muscles and make them more susceptible to attack from the immune system. Iron deficiency can also reduce levels of acetylcholine, a neurotransmitter that helps with muscle contraction, which can further weaken the muscles and lead to myasthenia gravis. The best way to prevent this type of iron deficiency is to eat a balanced diet that includes plenty of iron-rich foods such as grass-fed meat and dark leafy greens.12
What Causes Myasthenia Gravis – Low Vitamin D Levels
Evidence suggests that low levels of vitamin D play a role in the development and progression of Myasthenia Gravis. Vitamin D helps regulate nerve-muscle communication and the immune system, both of which can be disrupted in myasthenia gravis.
Low levels of vitamin D have been linked with an increased risk of developing myasthenia gravis, as well as higher severity of symptoms. Additionally, research suggests that supplementing with vitamin D may improve symptoms in some individuals with myasthenia gravis. Therefore, maintaining adequate levels of vitamin D is beneficial in managing symptoms of myasthenia gravis.13
Read more about Vitamin D and how important it is in autoimmune conditions.
What Causes Myasthenia Gravis – Insulin Resistance
Research suggests that insulin resistance (IR) may be responsible for myasthenia gravis. Insulin resistance is when the body does not respond appropriately to insulin, which increases blood sugar levels and can cause hormonal imbalances. Studies have shown that there is an association between high levels of insulin in the blood and myasthenia gravis. It is believed that the increased insulin levels create an environment in which autoimmunity can occur, resulting in MG.
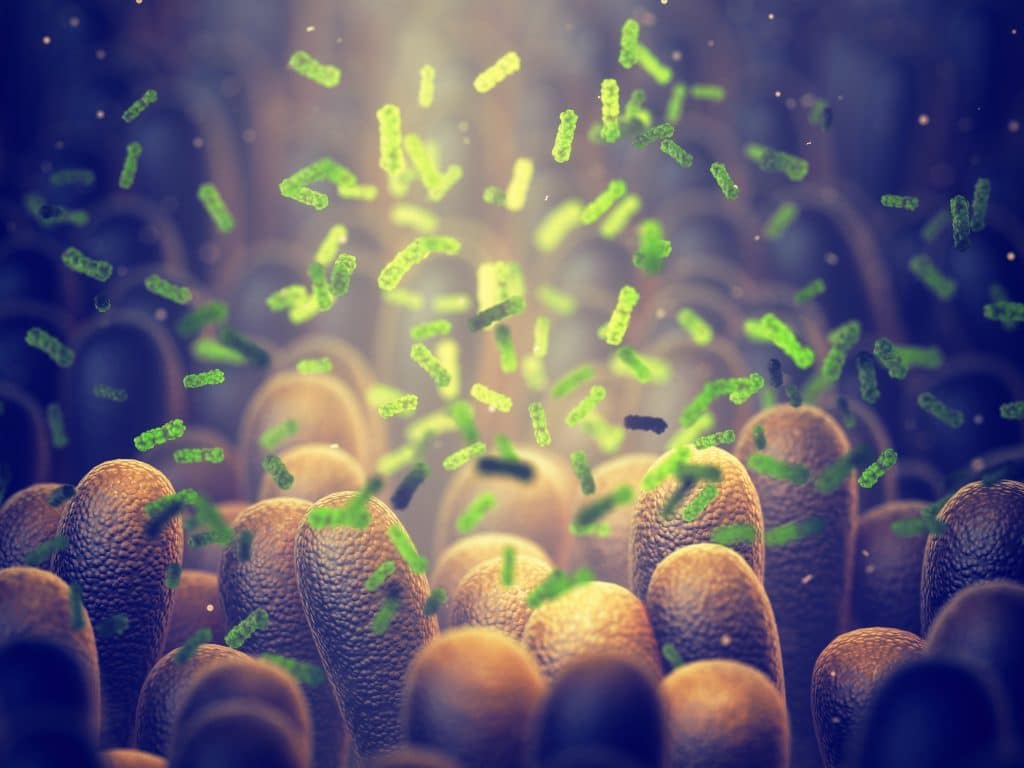
Myasthenia Gravis And The Microbiome
There is a strong link between autoimmune conditions and the microbiome. When the microbial balance is disrupted, the body’s natural defenses are weakened and it can become more susceptible to developing autoimmunity.
One area of investigation has focused on the role of the microbiome in Myasthenia Gravis, as alterations in gut microbiota composition have been documented in both human and animal models. Studies examining the gut microbiota profile in patients with Myasthenia Gravis have found differences when compared to healthy individuals.15 These results suggest that changes in the microbiome are an important factor in the development and progression of Myasthenia Gravis.16 17
Managing Myasthenia Gravis – Exercise
Exercise is an important part of managing Myasthenia Gravis. Exercise can help improve muscle strength, maintain mobility, and reduce fatigue. Studies have indicated that aerobic activity like walking, biking, swimming, or jogging can be beneficial for MG patients.18 Ideally, aim for at least 150 minutes of exercise weekly to improve muscle strength and function.19
What Causes Myasthenia Gravis – And How To Manage It
Now that you know the factors that cause Myasthenia Gravis, an improvement in lifestyle and a reduction in toxin exposure can reduce the risk of developing this disease. While there is no known cure, exercise, a healthy diet that includes sufficient iron-rich foods, and sufficient vitamin D intake all make managing Myasthenia Gravis more bearable.
References
1 Myasthenia Gravis. (2023). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/myasthenia-gravis
2 Claytor B, Cho SM, Li Y. Myasthenic crisis. Muscle Nerve. 2023 Apr 28. doi: 10.1002/mus.27832. Epub ahead of print. PMID: 37114503.
3 Liu FC, Kuo CF, See LC, Tsai HI, Yu HP. Familial aggregation of myasthenia gravis in affected families: a population-based study. Clin Epidemiol. 2017 Nov 2;9:527-535. doi: 10.2147/CLEP.S146617. PMID: 29138598; PMCID: PMC5679568.
4 Koneczny I, Herbst R. Myasthenia Gravis: Pathogenic Effects of Autoantibodies on Neuromuscular Architecture. Cells. 2019 Jul 2;8(7):671. doi: 10.3390/cells8070671. PMID: 31269763; PMCID: PMC6678492.
5 Avidan N, Le Panse R, Berrih-Aknin S, Miller A. Genetic basis of myasthenia gravis – a comprehensive review. J Autoimmun. 2014 Aug;52:146-53. doi: 10.1016/j.jaut.2013.12.001. Epub 2013 Dec 19. PMID: 24361103.
6 Bubuioc AM, Kudebayeva A, Turuspekova S, Lisnic V, Leone MA. The epidemiology of myasthenia gravis. J Med Life. 2021 Jan-Mar;14(1):7-16. doi: 10.25122/jml-2020-0145. PMID: 33767779; PMCID: PMC7982252.
7 Tanovska N, Novotni G, Sazdova-Burneska S, Kuzmanovski I, Boshkovski B, Kondov G, Jovanovski-Srceva M, Kokareva A, Isjanovska R. Myasthenia Gravis and Associated Diseases. Open Access Maced J Med Sci. 2018 Mar 5;6(3):472-478. doi: 10.3889/oamjms.2018.110. PMID: 29610603; PMCID: PMC5874368.
8 Amin S, Aung M, Gandhi FR, Pena Escobar JA, Gulraiz A, Malik BH. Myasthenia Gravis and its Association With Thyroid Diseases. Cureus. 2020 Sep 4;12(9):e10248. doi: 10.7759/cureus.10248. PMID: 33042687; PMCID: PMC7536109.
9 Wang Y, Qi G, Yang Y. Analysis of clinical features of myasthenia gravis complicated with hyperthyroidism. Pak J Med Sci. 2022 Mar-Apr;38(3Part-I):530-535. doi: 10.12669/pjms.38.3.4656. PMID: 35480500; PMCID: PMC9002454.
10 Nemet AY, Kaiserman I, Mimouni M, Segal O, Vinker S. High prevalence of myasthenia gravis among rural adult populations. J Clin Neuromuscul Dis. 2014 Dec;16(2):47-50. doi: 10.1097/CND.0000000000000054. PMID: 25415514.
11 Samih M, Ahami AOT. Excessive Pesticide Use Likely to Cause the Onset of Myasthenia Gravis in the Moroccan Agricultural Population. Pak J Biol Sci. 2020 Jan;23(7):917-921. doi: 10.3923/pjbs.2020.917.921. PMID: 32700839.
12 Huang P. The relationship between serum iron levels and AChR-Ab and IL-6 in patients with myasthenia gravis. Eur Rev Med Pharmacol Sci. 2023 Jan;27(1):98-102. doi: 10.26355/eurrev_202301_30857. PMID: 36647855.
13 Bonaccorso G. Myasthenia Gravis and Vitamin D Serum Levels: A Systematic Review and Meta-analysis. CNS Neurol Disord Drug Targets. 2023;22(5):752-760. doi: 10.2174/1871527321666220707111344. PMID: 35796450.
14 Li LJ, Guan YZ, Lü F, Song YW, Xu XJ, Jiang Y, Wang O, Xia WB, Xing XP, Li M. [Glucose and lipid metabolic disorders in myasthenia gravis patients and its mechanisms]. Zhonghua Yi Xue Za Zhi. 2018 Feb 27;98(8):581-586. Chinese. doi: 10.3760/cma.j.issn.0376-2491.2018.08.005. PMID: 29534385.
15 Schirò G, Iacono S, Balistreri CR. The Role of Human Microbiota in Myasthenia Gravis: A Narrative Review. Neurol Int. 2023 Mar 10;15(1):392-404. doi: 10.3390/neurolint15010026. PMID: 36976669; PMCID: PMC10053295.
16 Rinaldi E, Consonni A, Guidesi E, Elli M, Mantegazza R, Baggi F. Gut microbiota and probiotics: novel immune system modulators in myasthenia gravis? Ann N Y Acad Sci. 2018 Feb;1413(1):49-58. doi: 10.1111/nyas.13567. Epub 2018 Jan 17. PMID: 29341125.
17 Thye AY, Law JW, Tan LT, Thurairajasingam S, Chan KG, Letchumanan V, Lee LH. Exploring the Gut Microbiome in Myasthenia Gravis. Nutrients. 2022 Apr 14;14(8):1647. doi: 10.3390/nu14081647. PMID: 35458209; PMCID: PMC9027283.
18 Rahbek MA, Mikkelsen EE, Overgaard K, Vinge L, Andersen H, Dalgas U. Exercise in myasthenia gravis: A feasibility study of aerobic and resistance training. Muscle Nerve. 2017 Oct;56(4):700-709. doi: 10.1002/mus.25552. Epub 2017 Mar 24. PMID: 28085204.
19 Gilhus NE. Physical training and exercise in myasthenia gravis. Neuromuscul Disord. 2021 Mar;31(3):169-173. doi: 10.1016/j.nmd.2020.12.004. Epub 2020 Dec 24. PMID: 33461846.




