Toxins Cause Inflammatory Disease – Toxins Drive Cellular Membrane Inflammation
It has long been known that toxins cause inflammatory disease through the production of reactive oxygen species (ROS). The resulting inflammation causes macrophages, immune cells that have a crucial role in the innate immune response, to signal their mitochondria to stop producing ATP and instead churn out toxic compounds. Furthermore, inflammation of the cellular membrane causes nutrient and waste transport issues, along with hormone resistance.
This detrimental combination results in cells that struggle to transport substances across the cellular membrane and mitochondria that aren’t producing sufficient energy. Without enough ATP, cells are unable to produce sufficient glutathione to deal with cellular metabolic waste and toxic buildup. This is how toxin-induced inflammation leads to hepatitis, nephritis, scleroderma, lupus, atherosclerosis, rheumatoid arthritis, asthma, inflammatory bowel disease, and so on.
Toxins Cause Inflammatory Disease By Activating Reactive Oxygen Species (ROS)
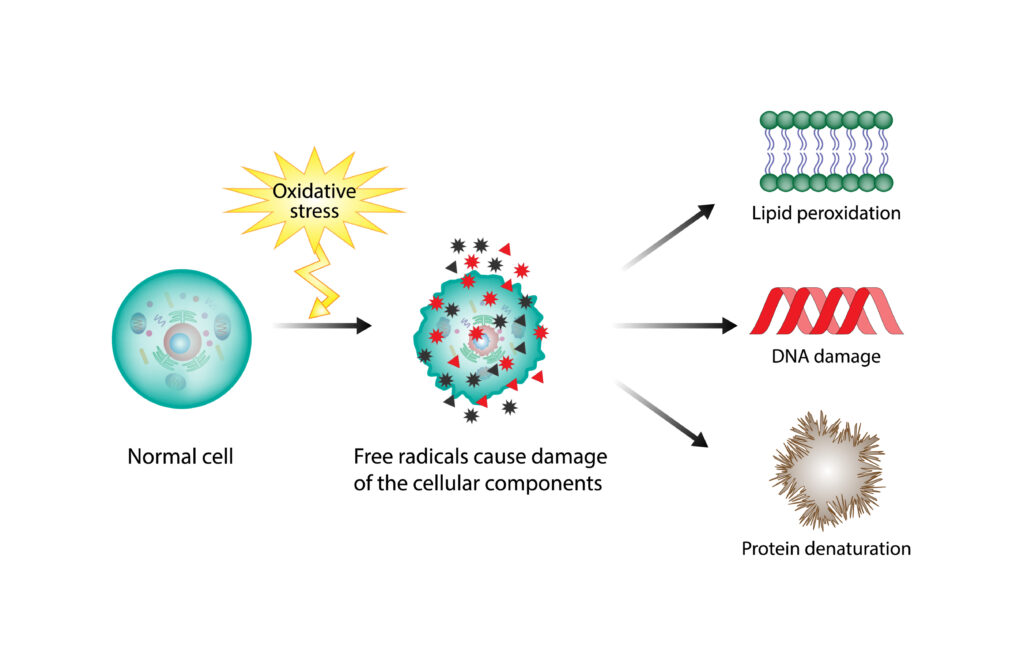
Toxins such as heavy metals, pesticides, and air pollutants promote the generation of reactive oxygen species (ROS) through cytochrome P4502E1 activation, leading to inflammatory diseases. ROS are highly reactive molecules that cause damage to cells and tissues when present in excessive amounts.1
One way toxins activate ROS is by disrupting normal cellular processes. For example, heavy metals like lead and mercury inhibit enzymes involved in antioxidant defense, which lead to an accumulation of ROS in cells.
Toxins also directly induce the production of ROS through various mechanisms. Some toxins contain free radicals or other reactive molecules that directly damage cells. Other toxins bind to receptors on cell membranes and stimulate the production of inflammatory mediators, which in turn activate ROS-producing enzymes.
The excessive levels of ROS produced by toxins cause damage to various cellular components, including DNA, proteins, and lipids. This oxidative damage is linked to a wide range of inflammatory diseases.2
Toxins Cause Inflammatory Disease – Toxins Affect The Macrophages’ Mitochondria
Toxins contribute to inflammatory diseases by compromising the body’s ability to regulate inflammation. Chronic exposure to toxins has been shown to alter the function of immune cells responsible for controlling inflammation, leading to an imbalance in the body’s natural inflammatory response.
Macrophages play a crucial role in this process by recognizing and responding to toxins. When they encounter toxins, macrophages activate their defense mechanisms, including phagocytosis (ingestion of foreign particles) and cytokine production (inflammatory signaling). These actions help to remove the toxins and prevent further damage to the body.
However, long-term elevated levels of macrophages induce systemic inflammation. When a certain substance called lipopolysaccharide (LPS) stimulates macrophages, they change the way they produce energy from ATP to glycolysis. This also causes an increase in succinate levels.
High levels of succinate leads to increased production of reactive oxygen species (ROS) in the mitochondria, which triggers a pro-inflammatory response. Essentially, macrophages change their metabolism to produce more ROS instead of energy when stimulated by LPS.3
The Link Between Cellular ATP Levels And Glutathione Production
Glutathione, also known as GSH, is a powerful antioxidant that plays an important role in maintaining cellular health. It is involved in various physiological processes and helps protect cells from damage caused by reactive oxygen species (ROS) and free radicals.4
One of the key factors that contributes to glutathione production is cellular ATP levels. ATP, or adenosine triphosphate, is often referred to as the “energy currency” of cells because it provides the energy needed for essential cellular processes.
Studies have shown that there is a direct link between cellular ATP levels and glutathione production. This is because the production of glutathione requires ATP as a source of energy.5 When cellular ATP levels are low, the production of glutathione is reduced. This leads to an imbalance between antioxidants and ROS, resulting in oxidative stress and damage to cells.
On the other hand, when cellular ATP levels are high, the production of glutathione is increased. This helps maintain a healthy balance between antioxidants and ROS, protecting cells from oxidative damage. Therefore, restoring optimal levels of ATP is crucial for the production of glutathione and cellular detoxification.6

Toxins Cause Inflammatory Disease By Inducing Cellular Membrane Inflammation
Toxins not only cause chronic inflammation throughout the body, but they also drive cellular membrane inflammation. This causes the cellular membrane to become less permeable and make it harder for nutrients to be shuttled into cells and waste products to be excreted.7
Think of each cell as a city surrounded by a wall. If the entrances to the city are blocked for whatever reason, the city will fill up with garbage and no new raw materials will be able to enter. Eventually, the city becomes a cesspool of filth and the inhabitants end up starving because there is no food coming in. In the same way, cellular membrane inflammation causes cells to fill up with metabolic waste products and the materials that are required for adequate cellular function and ATP synthesis are not replenished.
Cellular Membrane Inflammation And Hormone Resistance
Cellular membrane inflammation also causes integral membrane proteins like hormone receptors to change shape. The specific shape of a hormone receptor allows hormones to dock and drive cellular processes much like a key in a lock. When these hormone receptors change shape, the hormone doesn’t fit or it doesn’t function efficiently like it used to.
When hormones are unable to connect to cellular membrane receptors, it is called hormone resistance. Cellular membrane inflammation is what is driving the epidemic of hormone resistance, whether that be thyroid, estrogen, testosterone, insulin, or leptin resistance.8
When dealing with hormone resistance, the common practice is to simply give more hormones, but the problem isn’t that there aren’t enough hormones, but rather, they are unable to fit into hormone receptors. The holistic solution to dealing with hormone resistance is to optimize cellular function and downregulate cellular membrane inflammation so hormone receptors work as designed.
Toxins Cause Inflammatory Disease So We Must Remove Toxins To Resolve The Issue
Since toxins cause inflammatory disease, the solution all comes down to removing these toxins. However, it isn’t quite as simple as only removing toxins, as we must also repair the damage caused by these toxins so cellular function returns to normal.
In my own health struggles with mercury toxicity, I developed something I call the 5Rs for identifying toxins, removing them from the cells, and excreting them from the body for good.
Read more about how I overcame my health battle and developed the 5Rs.
5Rs – Addressing The Cause Of Inflammatory Disease
The first step, R1, involves identifying and removing the source of toxicity in our lives. This could include sources such as mercury fillings or other environmental factors that continue to poison our bodies.
Next, R2 focuses on regenerating the cellular membrane which as we discussed earlier is inflamed due to toxins like mercury. In addition to preventing important nutrients from entering cells and waste products from leaving, it also changes epigenetic expression which we will discuss in R5.
R3 is all about restoring cellular ATP production. By opening up detox pathways and supporting cellular function, we increase ATP production and also promote the production of glutathione so we can finally remove toxins from the cells.9
In R4, we address downregulating cellular membrane inflammation through targeted nutraceuticals. Unfortunately, removing toxins doesn’t immediately decrease inflammation, as a complex cycle called the NO/ONOO cycle maintains it. Thus, we use specific compounds to finally put an end to this inflammation.10
Finally, R5 involves restoring methylation through the use of methyl donors. Studies have identified specific genes involved in the inflammatory response that are regulated by methylation. For example, certain cytokines such as TNF-α and IL-6 have been found to be under epigenetic control through methylation. Additionally, studies have shown that changes in methylation levels influence the production of pro-inflammatory molecules like prostaglandins and leukotrienes, further contributing to the inflammatory response.11 12 13
Heavy metals disrupt methylation patterns and prevent proper detoxification so providing cells with sufficient methyl groups helps remove toxins and optimize gene expression. This allows us to turn off the genes that code for inflammatory diseases.

The 5Rs upregulates cellular function, enabling us to finally remove built up toxins from the cells and push them into the extracellular space. From there, chelating agents bind to them and move them to the liver.
When in the liver, toxins enter the bile and are one step closer to being completely excreted from the body. However, creating bile is energy intensive so the body typically reabsorbs it to use it again and again. This is why we use binders to pull toxins from the bile so they are finally excreted from the body, thereby avoiding autointoxication.14 15
This may all seem confusing at first which is why I encourage you to learn more about the 5Rs by joining me in my free webinar where I will answer all your questions.
Toxins Cause Inflammatory Disease – Toxins Drive Cellular Membrane Inflammation
Toxins cause inflammatory disease from multiple different angles. First, toxins produce reactive oxygen species. Secondly, toxins cause systemic, chronic inflammation that causes macrophages to downregulate ATP production and instead create toxic compounds that further exacerbate inflammation.
Next, toxins cause cellular membrane inflammation that hinders cellular function and results in hormone resistance. The end result is that toxin-induced inflammation is the driving cause behind a wide range of degenerative disorders and inflammatory diseases.
To learn even more about removing toxins from the cells and optimizing cellular function to get to the core cause of inflammatory disease, join me in my free webinar or read more about what toxins cause autoimmune conditions.
References
1 Parke DV, Parke AL. Chemical-induced inflammation and inflammatory diseases. Int J Occup Med Environ Health. 1996;9(3):211-7. PMID: 8972163.
2 Forrester SJ, Kikuchi DS, Hernandes MS, Xu Q, Griendling KK. Reactive Oxygen Species in Metabolic and Inflammatory Signaling. Circ Res. 2018 Mar 16;122(6):877-902. doi: 10.1161/CIRCRESAHA.117.311401. PMID: 29700084; PMCID: PMC5926825.
3 Mills, E. L., Kelly, B., Logan, A., Costa, A. S., Varma, M., Bryant, C. E., Tourlomousis, P., Däbritz, J. H. M., Gottlieb, E., Latorre, I., Corr, S. C., McManus, G., Ryan, D., Jacobs, H. T., Szibor, M., Xavier, R. J., Braun, T., Frezza, C., Murphy, M. P., & O’Neill, L. A. (2016). Succinate dehydrogenase supports metabolic repurposing of mitochondria to drive inflammatory macrophages. Cell, 167(2), 457-470.e13. https://doi.org/10.1016/j.cell.2016.08.064
4 Kwon DH, Cha HJ, Lee H, Hong SH, Park C, Park SH, Kim GY, Kim S, Kim HS, Hwang HJ, Choi YH. Protective Effect of Glutathione against Oxidative Stress-induced Cytotoxicity in RAW 264.7 Macrophages through Activating the Nuclear Factor Erythroid 2-Related Factor-2/Heme Oxygenase-1 Pathway. Antioxidants (Basel). 2019 Apr 1;8(4):82. doi: 10.3390/antiox8040082. PMID: 30939721; PMCID: PMC6523540.
5 Pizzorno J. Glutathione! Integr Med (Encinitas). 2014 Feb;13(1):8-12. PMID: 26770075; PMCID: PMC4684116.
6 Pastore A, Federici G, Bertini E, Piemonte F. Analysis of glutathione: implication in redox and detoxification. Clin Chim Acta. 2003 Jul 1;333(1):19-39. doi: 10.1016/s0009-8981(03)00200-6. PMID: 12809732.
7 Ammendolia, D.A., Bement, W.M. & Brumell, J.H. Plasma membrane integrity: implications for health and disease. BMC Biol 19, 71 (2021). https://doi.org/10.1186/s12915-021-00972-y
8 Straub RH. Interaction of the endocrine system with inflammation: a function of energy and volume regulation. Arthritis Res Ther. 2014 Feb 13;16(1):203. doi: 10.1186/ar4484. PMID: 24524669; PMCID: PMC3978663.
9 Zolkipli-Cunningham Z, Falk MJ. Clinical effects of chemical exposures on mitochondrial function. Toxicology. 2017 Nov 1;391:90-99. doi: 10.1016/j.tox.2017.07.009. Epub 2017 Jul 27. PMID: 28757096; PMCID: PMC6078194.
10 Pall M. L. (2013). The NO/ONOO-cycle as the central cause of heart failure. International journal of molecular sciences, 14(11), 22274–22330. https://doi.org/10.3390/ijms141122274
11 Dhar GA, Saha S, Mitra P, Nag Chaudhuri R. DNA methylation and regulation of gene expression: Guardian of our health. Nucleus (Calcutta). 2021;64(3):259-270. doi: 10.1007/s13237-021-00367-y. Epub 2021 Aug 16. PMID: 34421129; PMCID: PMC8366481.
12 Calle-Fabregat C, Morante-Palacios O, Ballestar E. Understanding the Relevance of DNA Methylation Changes in Immune Differentiation and Disease. Genes (Basel). 2020 Jan 18;11(1):110. doi: 10.3390/genes11010110. PMID: 31963661; PMCID: PMC7017047.
13 Xia, T., Fu, S., Yang, R. et al. Advances in the study of macrophage polarization in inflammatory immune skin diseases. J Inflamm 20, 33 (2023). https://doi.org/10.1186/s12950-023-00360-z
14 Sears ME. Chelation: harnessing and enhancing heavy metal detoxification–a review. ScientificWorldJournal. 2013 Apr 18;2013:219840. doi: 10.1155/2013/219840. PMID: 23690738; PMCID: PMC3654245.
15 Ko CW, Schulte SJ, Lee SP. Biliary sludge is formed by modification of hepatic bile by the gallbladder mucosa. Clin Gastroenterol Hepatol. 2005 Jul;3(7):672-8. doi: 10.1016/s1542-3565(05)00369-1. PMID: 16206500.
Disclaimer: All rights reserved. Information provided is for general purposes and not intended to provide medical advice, diagnosis, or treatment. Consult your healthcare professional for medical concerns. About Dr. Pompa




